Many men notice fullness or enlargement in the chest area and wonder whether it’s gynecomastia or just excess chest fat. While both can look similar, they have different causes and treatment approaches. Understanding the difference is the first step toward choosing the right solution and setting realistic expectations.
This self-check guide explains what gynecomastia is, why it’s often called “man boobs,” how to assess your symptoms, possible contributing factors, and when medical evaluation or treatment may be considered.
What Is Gynecomastia? Why Is Gynecomastia Commonly Called “Man Boobs”?
Gynecomastia is a medical condition characterized by the enlargement of male breast tissue, often caused by a hormonal imbalance between estrogen and testosterone. Unlike fat accumulation, gynecomastia involves the growth of glandular tissue, which does not respond well to diet or exercise alone.
The condition can affect one or both sides of the chest and may occur at different life stages, including adolescence, adulthood, or later in life.
The term “man boobs” is a non-medical phrase used to describe the appearance of a fuller or breast-like chest in men. While chest fat from weight gain can create a similar look, gynecomastia often feels firmer and more localized beneath the nipple area. This overlap in appearance is why the two conditions are frequently confused.
Hormone-Related Causes of Gynecomastia
Hormone-related factors are one of the most common contributors to gynecomastia in men. Certain hormone-related medications and substances can disrupt the natural balance between testosterone and estrogen in the body.
For example, testosterone-related medications, anabolic steroids, and substances sometimes used for bodybuilding may increase hormone levels initially but can ultimately lead to suppression of natural testosterone production. This imbalance may result in relatively higher estrogen activity, which can contribute to the development of gynecomastia.
Similarly, anti-androgen medications, such as those used in the treatment of prostate conditions or sometimes prescribed for hair loss, work by blocking or reducing the effect of testosterone. This reduction can allow estrogen to have a stronger influence, increasing the likelihood of breast tissue enlargement. Certain antipsychotic and antidepressant medications may also affect hormone regulation and have been associated with gynecomastia in some individuals.
Overall, taking hormone-related medications can lead to an imbalance between estrogen and testosterone levels, where testosterone is reduced or blocked and estrogen activity becomes more prominent, potentially contributing to gynecomastia.
Pubertal Gynecomastia: What’s Normal?
Gynecomastia during puberty is common and usually temporary. Studies suggest that 60–70% of adolescent boys experience some degree of breast enlargement during puberty. This occurs due to temporary hormonal fluctuations, where estrogen and testosterone levels may be briefly out of balance.
Pubertal gynecomastia typically begins between the ages of 11 and 14, often peaks during mid-puberty, and gradually reduces over time. In many cases, it resolves on its own within 6 to 18 months, though for some individuals, it may take up to two years to subside.
Medical evaluation may be considered if pubertal gynecomastia:
- Persists beyond two years
- Continues into late adolescence
- Is painful or tender
- Occurs predominantly on one side
- Appears to be increasing in size
Gynecomastia vs. Chest Fat: A Step-by-Step Self-Check
A self-check can help you become more aware of changes in your chest, but it cannot confirm a diagnosis or determine the grade of gynecomastia.
To perform a basic self-check:
- Stand in front of a mirror and observe the chest for asymmetry or swelling
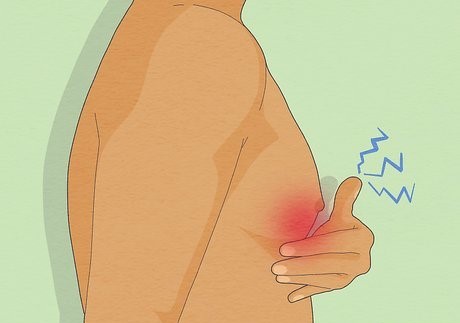
- Gently press beneath the nipple using your thumb and index finger
- A round, firm, or rubbery lump under the nipple may suggest glandular tissue
- Soft, diffuse tissue is more commonly associated with fat
- Gynecomastia can sometimes be one-sided
- Pain or tenderness may also be present in some cases
It is important to note that self-checking cannot reliably distinguish between fat and glandular tissue, determine whether the condition is early or advanced, or assess the severity. A proper medical evaluation is necessary for accurate diagnosis and guidance.
How Gynecomastia Is Identified Clinically
The identification and assessment of gynecomastia are based on several physical factors rather than appearance alone. Doctors evaluate the amount of glandular breast tissue, the presence of fat, and whether there is excess or loose skin.
One commonly used system is the Simon’s classification, which categorizes gynecomastia based on tissue volume and skin excess:
- Grade 1: Small enlargement without excess skin
- Grade 2A: Moderate enlargement without skin excess
- Grade 2B: Moderate enlargement with mild excess skin
- Grade 3 (often referred to as Grade 4): Marked enlargement with significant skin excess and sagging
In addition to grading, clinicians may also assess:
- Overall breast volume
- Presence of skin folding or sagging
- Skin elasticity
- Position of the nipple and areola
These factors help determine the nature and extent of the condition and guide further management.
What Factors May Contribute to Gynecomastia?
Several factors may play a role in the development of gynecomastia, including:
- Hormonal changes or imbalances
- Certain medications or supplements
- Underlying medical conditions
- Weight fluctuations
- Alcohol or substance use
- Genetic predisposition
In some cases, the cause may not be clearly identifiable.
When Is Surgery Considered?
Gynecomastia removal surgery may be considered when:
- The condition has persisted for an extended period
- Non-surgical approaches have not improved the appearance
- Physical discomfort or emotional distress is present
- Glandular tissue is confirmed by medical evaluation
Surgical treatment focuses on male boobs removal through gland excision, liposuction, or a combination, depending on the individual case.
What to Know About Gynecomastia Recovery Time
Gynecomastia recovery time varies based on the extent of the procedure and individual healing factors. Most patients can return to light activities within a few days, while full recovery may take several weeks. Swelling and firmness can persist temporarily and gradually improve with time and proper post-procedure care.
How to Choose the Right Gynecomastia Doctor
Search using the keyword “gynecomastia doctors near me” to find the best doctors for gynecomastia. While choosing the right one, consider the following factors:
- Board certification and relevant surgical training
- Experience specifically with gynecomastia cases
- Before-and-after case examples
- Transparent discussion of risks, recovery, and outcomes
- Access to proper surgical facilities and follow-up care
Choosing the right doctor is essential for safety, realistic expectations, and informed decision-making.
Cost Considerations
The gynecomastia operation price can vary based on the complexity of the condition, surgical technique used, facility fees, and geographic location. A personalized consultation is necessary to determine accurate costs and suitable treatment options.
Final Thoughts
Chest fullness in men can be caused by different factors, and distinguishing between chest fat and gynecomastia is not always straightforward. A proper medical evaluation is the most reliable way to understand your condition and explore appropriate options. With the right information and professional guidance, you can make confident, informed decisions about your care.